Our Locations
Our Clinics
Gurugram
Kashmir
Dhadri
How to Choose a Right IVF Centre
Choosing the right IVF clinic is a pivotal decision for couples embarking on their fertility journey. With numerous options available, it’s essential to consider several factors to ensure the best possible outcome. Here’s a guide to help you navigate this critical choice.
Success Rates: Look for clinics with proven and consistent success rates, which indicate their expertise and effectiveness in treatments.
Accreditation and Facilities: Ensure the clinic is accredited under the Assisted Reproductive Technology (Regulation) Act, 2021. Level 1 or Level 2 ART clinics should meet stringent standards for equipment and infrastructure.
Fertility Specialists: Check that the clinic has experienced fertility specialists with expertise in reproductive endocrinology and a proven track record in treating complex issues

Patient Testimonials
Why Choose Us
Choosing the right fertility clinic is crucial for starting your family. At Birla Fertility & IVF, we offer personalised care with expert specialists guiding you every step of the way. Our advanced labs and outstanding success rates have helped over 2,30,000 patients achieve their dream of parenthood.
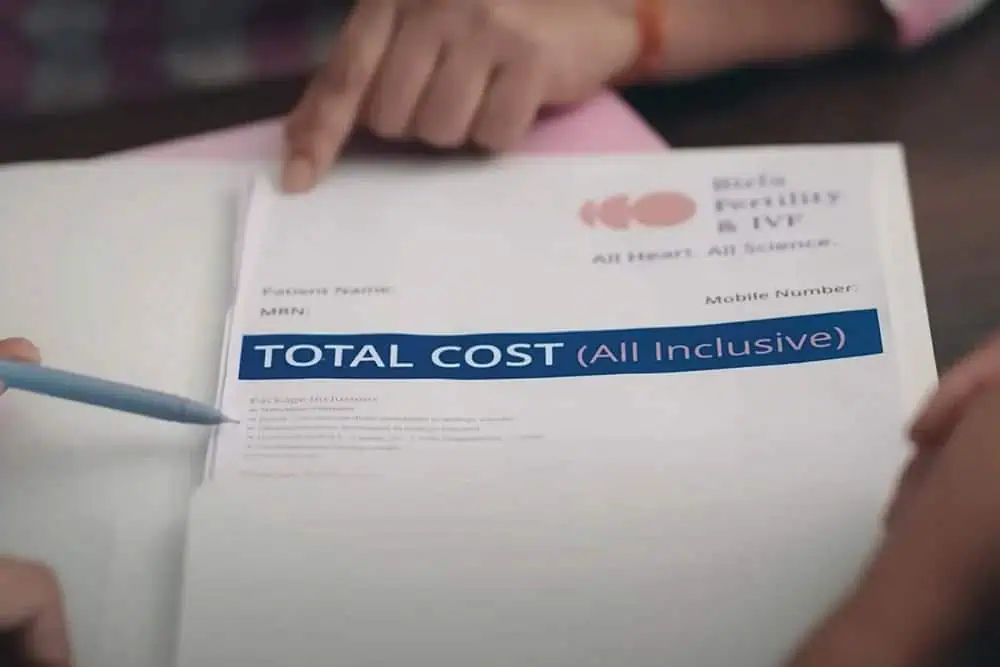
100% Transparent & Affordable Pricing
We are committed to making world-class fertility treatments affordable and accessible. We offer fixed price all-inclusive packages and 0% EMI

95% Patient Satisfaction Score
We offer personalized treatment plans and comprehensive fertility services, ensuring exceptional fertility care under one roof.
